Ketamine-Assisted Therapy
Experience lasting, full-body and mind healing
Whether you realize it or not, you have likely experienced some degree of trauma in your life. This can be a physical, mental or emotional response left in the body or mind after an impactful experience.
Though many types of trauma exist, the result is typically the same – a negative impact on long-term physical and mental health.
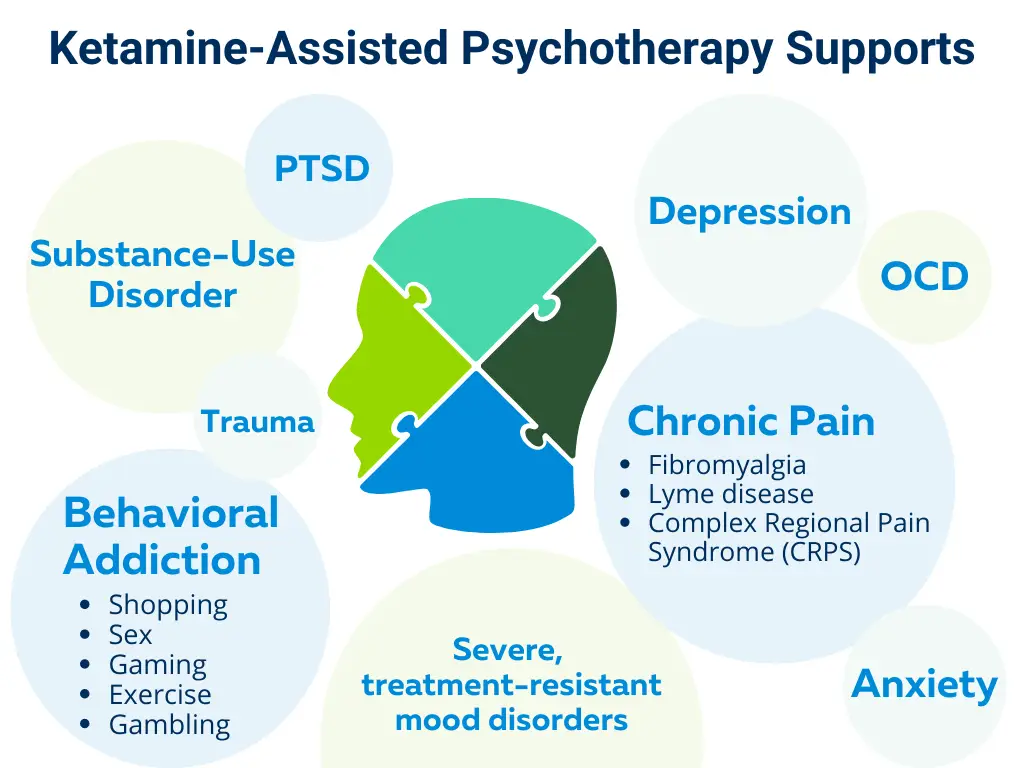
Left unaddressed, trauma may lead to unhealthy behavior patterns, low self-esteem, and symptoms of depression, anxiety, OCD, PTSD, and more.
However, there is hope through an integrative approach with ketamine-assisted therapy.
What is Ketamine Infusion therapy?
Ketamine is a safe, legal medication originally used as a dissociative anesthetic.
As a dissociative, it alters sensory perception, physical senses like sight and sound, and creates feelings of being in an observing point of view of yourself and your environment. As an anesthetic, it temporarily dulls sensation, including pain, by temporarily softening nervous system responses.
When used therapeutically, ketamine creates an altered state of consciousness that promotes a sense of calm, openness and vulnerability, and temporarily softens the ego.
Conditions Treated with Ketamine Infusion Therapy
To learn more about ketamine therapy:
What makes Forum Health different?
Nuanced Dosing:
We are not a one-size-fits-all clinic. We consider your age, metabolism, lifestyle, and medications to determine the appropriate dose for your session. We believe this personal approach is the key to long-term healing.
Ensured Comfort:
Experienced medical technicians supervise the infusion to ensure your safety and comfort the entire time, so that you full benefits of your session in a comfortable environment.
Expert Guides:
Highly trained, trauma-informed guides are in the room, physically or virtually, to lead you through the session and to integrate the traumas and information that comes up. A ketamine experience without integration is just an experience. The long-term benefits come from applying new insight into your life.
Integrative Approach:
We take an integrative, root-cause approach to healing the mind-body connection to promote full-body healing.
Read What Patients Are Saying
How do I know if ketamine-assisted therapy is right for me?
We have found this therapy is especially useful if you:
- Are not functioning optimally mentally and emotionally
- Are stuck in a negative loop or cycle you can’t escape
- Are repeating unproductive patterns of behavior
- Recognize unhealthy coping mechanisms:
- Avoidance, procrastination or low motivation
- Excessive sleep or overworking
- Unhealthy relationship to drugs, alcohol or other substances
- Excessive exercise or sex
- Impulsive behavior, unhealthy risk-taking
- Changes in eating habits
What Can I Expect From My Session?
- Your session will take place in relaxing setting with a comfortable reclining chair, soft lighting, blanket and eye mask. Our goal is to make you feel as calm and at ease as possible.
- A licensed medical technician will take your vitals and then administer a prescribed low dose of ketamine. You will begin to experience a sense of “one-ness” and a kind of third-party objectivity sets in. Many patients report experiencing a heavy body sensation, followed by feeling light as a feather and the relief of any pain in the body.
- During your session, a therapist is present to help you work through anything that arises to facilitate healing including subconscious negative mindsets, memories, images, or feelings.
- As the session ends, you’ll be guided by the therapist to slowly transition to a baseline state of consciousness. It is this integration of experience that fosters long- term healing. Patients will start to feel “normal” 30 minutes after the session ends, however we suggest having someone pick you up from the clinic.

Want to learn more?
Watch Julie Hamilton, NP and Andrew Petersen, DO discuss how ketamine-assisted therapy is the new legal psychedelic changing mental health
Schedule Your Ketamine-Assisted Therapy Session
Frequently Asked Questions
Contact clinic for pricing details and package options.
Many find ketamine infusions relaxing and peaceful with visuals of colors, geometric patterns, and synesthesia between music and your senses. It is also not uncommon for patients to describe having an out-of-body experience during their session.
At Forum Health, we use the lowest possible therapeutic doses which typically allows recall of the entire session
After a Ketamine session, patients typically emerge with a newfound sense of wholeness, calm, and empowerment to live life to its fullest. Old habits, unhealthy coping mechanisms, and limiting thought patterns are left behind.
Current pharmaceutical options for depression and anxiety tend to lose their efficacy over time and require either an increase in dosage or the addition of another adjunct medication which can come with adverse side effects.
We do not accept insurance at this time. However, we can provide a super bill, including procedure codes, that you may submit to your insurance company for possible reimbursement. We are unable to guarantee reimbursement for services rendered.
We offer a comprehensive, one hour intake appointment with our nurse practitioner prior to starting ketamine therapy. This appointment includes a comprehensive medical history and physical exam to identify and address any potential health issues prior to starting ketamine therapy. Strict contraindications: allergy to ketamine, recent TBI, history of psychosis, bipolar disorder with active mania. Relative contraindications: severe respiratory compromise, personality disorders, severe kidney disease, severe liver disease.
Ketamine therapy has demonstrated to be effective for treatment resistant depression, anxiety, OCD and PTSD. Ketamine therapy is often effective when SSRIs (antidepressants) have failed because ketamine works differently in the body. Antidepressants work on neurotransmitters such as serotonin, dopamine, norepinephrine. Conversely, Ketamine binds to a receptor in the brain called a NMDA (N-methyl-D-aspartate). This binding blocks a part of the glutaminergic system called glutamate. Glutamate dysfunction has been correlated to mood disorders in clinical studies.
Every individual is unique and will therefore have a unique ketamine experience. However, you will likely experience a sensation of heaviness, or even decreased awareness of your body. Ketamine experiences are often filled with colors and geometric shapes, as well as a heightened awareness of sound and music. Additionally, time is experienced differently under the effects of ketamine. A 40-minute session may feel much longer. Your guide is present to help you interpret your experience. Several common descriptors of the ketamine experience include; “calm”, “one-ness”, and “peaceful”.
Here at Forum Health, we go above and beyond the industry standard to ensure your safety during infusion. We use the lowest possible therapeutic doses, which serves to nearly eliminate uncomfortable side effects. Also, you will be monitored throughout the entire session, using state-of-the-art medical equipment to ensure your well-being during infusion. Additionally, we provide a thorough, one-hour medical intake prior to initiating therapy in order to identify and address any potential health risks before your first infusion.
Our trained technicians ensure your comfort, place your IV, and remain in the room for monitoring. The therapist remains chairside, either personally or remotely, during the therapy portion. As the infusion of medication comes to an end, your therapist will transition you through post-session integration.
*These statements have not been evaluated by the Food and Drug Administration. These products are not intended to diagnose, treat, cure or prevent any disease.


